
The following factors may contribute to the development of osteoarthritis of the knee joints:
- excessive physical activity that does not meet the age requirements, causing joint damage;
- sedentary lifestyle;
- received injuries in the area of the knee joints - dislocation of the knee, fractures, fractures and tears of the ligaments, damage to the body of the meniscus, severe falls on the knee, bruising;
- increase in body mass index, tearing of the meniscus, causing increased stress on the joints;
- heredity;
- arthritis or other joint diseases (inflammation can lead to the appearance of edema or accumulation of large amounts of synovial fluid in the joints, can lead to the destruction of cartilage tissue);
- metabolic disorders that cause the excretion of calcium from the body;
- any type of diabetes, hormonal disorders and other pathologies of the endocrine system;
- chronic or past diseases of inflammatory and infectious nature;
- impaired blood flow;
- lupus erythematosus, rheumatoid, gout and psoriatic pathologies, ankylosing spondylitis;
- straight legs, due to which the center of gravity changes and the load on the joint increases;
- nervous load and stressful situations.
Why Osteoarthritis of the Knee Joint Occurs
Often people themselves are to blame for the development of such a serious disease. Often, when pain appears in the knee joint, people ignore the painful sensations and simply prefer to go to the doctor to use any medication that masks the pain.
After a few years, you will still have to consult a specialist, because self-treatment with such a diagnosis will not work. However, the severity of osteoarthritis will be at least moderate. Ointments, intraarticular application of hyaluronic acid and prophylactic physical training are no longer enough, as they can be done in the early stages of the disease. It is likely that radical action is required, sometimes with the use of surgery.
Symptoms and diagnosis of osteoarthritis of the knee joints
The disease can be distinguished by the following symptoms:
- Pain syndrome. Painful feelings usually occur suddenly, but often with physical force, even if minor. Pain can have a different nature. At first they will be weak lumbago (unfortunately few people pay attention to them). Mild pain, which occurs only occasionally, can last for months or even years until the disease progresses to a more severe stage.
- Knee deformity. A similar symptom is characteristic of the later stages. And at the beginning of the development of osteoarthritis, the knee swells and swells a little.
- Appearance of dense formations on the posterior wall of the knee joints. Accumulation of large amounts of joint fluid in the cavity of the Baker cyst or in the joint itself.
- An acute crisis of the joints accompanied by pain.
- Decreased joint mobility. This is especially true in the later stages of osteoarthritis. In this situation, bending and stretching the knee causes severe pain, and in the final stages, movement is almost impossible.
REFERENCE! In a patient with osteoarthritis, gait changes: it is characterized by lowering and limping of the legs.
Pathogenesis of osteoarthritis of the knee joints
Specialists distinguish between primary and secondary osteoarthritis.
Primary arthrosis of the knee joints
The following processes are characteristic of primary gonarthrosis:
- Joint cartilage is constantly deteriorating and at the same time is able to regenerate rapidly. Under normal circumstances, these two processes must balance each other. With age, cartilage destruction occurs at the same rate, but recovery slows. The human mass plays an important role here. Indeed, if a person weighs 70 kg, then in 10 steps on one leg he will transfer 700 kg, and 120 kg - up to 1200 kg, which will be a significant load on the joints. therefore, the cartilage will wear out faster.
- It is important to remember: the joint is nourished with useful elements only when moving. A sedentary lifestyle slows down metabolic processes, so the necessary nutrients do not reach their destination.
- People whose parents suffer from this disease are more likely to develop gonarthrosis.
Secondary osteoarthritis of the knee joint
It develops for the following reasons:
- Numerous injuries. They will cause excessive stress on the cartilage in a person of any age. When any bone covered with cartilage is broken, violations called "steps" appear. In this area, now, with any movement, the joint wears out, causing osteoarthritis.
- Development of rheumatoid arthritis, Koenig's disease, the appearance of purulent inflammation in the joint area.
- Vascular dysfunction.
Classification and stages of development of osteoarthritis of the knee joints
Orthopedists divide gonarthrosis into stages on which further treatment of the disease depends. Of course, the course of treatment will also depend on other factors, such as the causes of the development, localization and nature of osteoarthritis.
IMPORTANT! Quality treatment can be prescribed by a doctor only after a thorough study of the disease. Self-administered therapy can only aggravate the health condition.
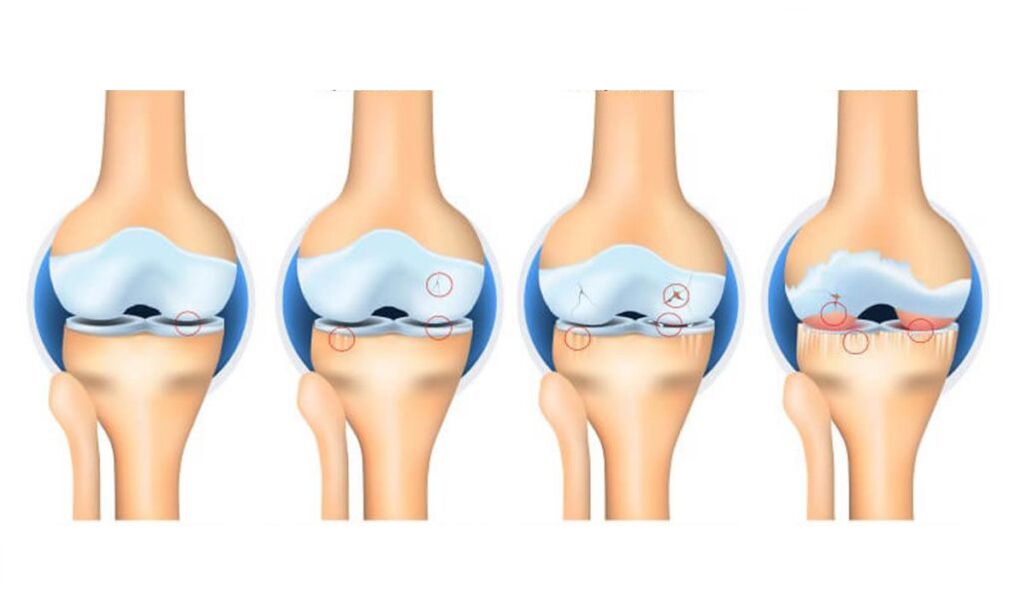
The main classification divides gonarthrosis into four stages of development:
- The initial stage. At this stage, the disease is just emerging. External symptoms are difficult to notice or absent, the shape of the joint is satisfactory. Symptoms include only mild discomfort or heaviness in the knee after long walks, as well as strong physical force. X-ray examination will give little information: X-ray can only show a slight narrowing of the joint space. Unfortunately, at this stage a person does not seek medical help due to the insignificance of symptoms.
- The second stage is characterized by noticeable pain syndrome, especially when walking and climbing stairs, as well as at night. The severity of the pain decreases at rest. Joint movement is difficult. While walking, you can hear the squeaking or creaking of the knees. X-rays show narrowing of the joint space, as well as osteophytes. The patient begins to stumble.
- When osteoarthritis progresses to the third stage, the pain syndrome will always be felt, even if it is inactive. Deformation and degeneration processes are irreversible. The distortion of the joint becomes apparent, the distance between the articular surfaces decreases significantly, and the number of osteophytes increases in size. Painful feelings now bother the patient even at complete rest. A person depends on outside support (walkers, sticks) and needs the help of other people. At this stage, conservative treatment is less effective.
- The fourth stage is characterized by constant debilitating pain. The number and size of osteophytic growths increase, cartilage is completely destroyed, the joint space is difficult to follow or disappear completely, and bones are severely deformed. Even weak movements become torture for the patient. At this stage of gonarthrosis, the patient is recognized as disabled. In the absence of surgery, the disease can lead to disability.
Complications of osteoarthritis of the knee joints
Advanced osteoarthritis can lead to dislocation and subluxation of the knee joint. With dislocation, the epiphysis of the femur extends completely outside the joint, making movement in the joint impossible and the axis of the foot shifting significantly to the side. Fortunately, such a negative variant of the disease is very rare.
Subluxation is more common. They are characterized by partial displacement of the joints relative to each other and a slight deviation of the tibial axis. In this condition, subluxations are accompanied by severe pain and joint dysfunction.
Neglect of the disease can lead to complete loss of functionality of the lower extremities.
ATTENTION! The habit of protecting a painful leg sometimes leads to deformation of the intervertebral discs and the appearance of hernias.
Consequences of neglected gonarthrosis
The advanced stage of gonarthrosis is almost always characterized by the following unpleasant symptoms:
- day and night pain that no painkiller can save;
- loss of support for a limb (it is impossible to stand or at least lean on a painful leg);
- immobilization of the articular block;
- open curvature of the bones around the knee;
- severe swelling around the affected area.
Methods of treatment of osteoarthritis of the knee joint
The treatment prescribed depends on the stage of the disease. There are several therapy options.
Hormones
These drugs are prescribed for severe exacerbations accompanied by synovitis and severe pain. Hormones are usually given by injection. The following medications are most commonly used:
- flosterone;
- Diprosfan;
- Hydrocortisone.
The course of hormone therapy is generally short, injections are given only during periods of severe exacerbation. Hormones are given on average once every 10 days.
Chondroprotectors
Chondroprotectors are prescribed in the early stages of the disease. This therapy is currently considered the most effective and safest: there are virtually no contraindications, and side effects are rarely seen.
The drugs are intended to restore cartilage tissue, improve metabolic processes, nourish cartilage tissue and protect it from further destruction. However, in the later stages of osteoarthritis, chondroprotectors are also weak.
This group of drugs is produced in the form of injections, ointments, gels, tablets.
Vasodilator drugs
These funds are needed to relieve spasm of small blood vessels, increase blood circulation and increase the supply of nutrients to the affected joint area. Vasodilators are prescribed together with chondroprotectors.
If articular fluid does not accumulate during gonarthrosis (no synovitis), it is recommended to use warming ointments.
Hyaluronic acid
Alternatively, this tool is called an intraarticular fluid prosthesis because the acid content is similar to that of intraarticular fluid. When the acid is injected into the joint, it forms a film that prevents strong cartilage friction during movement, affects the extracellular matrix, improves metabolic processes in the joint, and triggers the production of its own hyaluronic acid in the joint - that is. restores joint function, stops pathological processes that destroy cartilage. . . .
Acid treatment is prescribed only in case of exacerbation - synovitis is eliminated.
Physiotherapy
A course of physiotherapy exercises will give positive results only if it is prescribed by a doctor after a thorough study of the history of the disease, and all exercises are carried out under the supervision of a specialist.
Self-medication often leads to worsening of the joint condition. Exercise therapy is prescribed for the following purposes:
- slow down the development of stiffness;
- prevention of further destruction of cartilage tissue;
- Eliminate muscle spasms, causing pain.
Physiotherapy
Various procedures can be prescribed as additional therapy: electrophoresis, acupuncture, laser therapy, UHF, as well as diadynamic currents. Local massage will also give good results.
Physiotherapy aims to reduce the severity of pain, eliminate inflammation, normalize metabolic processes within the affected joint and restore normal function.
IMPORTANT! It is important to monitor the patient's diet and avoid strenuous physical exertion.
Forecast. Prophylaxis
With an advanced stage of the disease, the prognosis is disappointing. Therefore, even if there are minor symptoms of osteoarthritis, it is recommended to consult a doctor.
People at risk (the elderly, athletes, as well as overweight people) should follow the doctor's recommendations and follow the following rules:
- Eat right and manage your weight. Follow a weight loss diet if necessary.
- When playing sports, reduce the load on the joints, constantly monitor.
- Timely treatment of infectious diseases, prevention of their transition to a chronic stage.
- If possible, get enough rest and avoid stressful situations.
- Increase the body's protective functions (take vitamins on time, get nervous).
- Avoid hypothermia of the body, especially the lower extremities.

















































